Abstract
As the global population ages, it is critical to identify diets that, beyond preventing noncommunicable diseases, optimally promote healthy aging. Here, using longitudinal questionnaire data from the Nurses’ Health Study (1986–2016) and the Health Professionals Follow-Up Study (1986–2016), we examined the association of long-term adherence to eight dietary patterns and ultraprocessed food consumption with healthy aging, as assessed according to measures of cognitive, physical and mental health, as well as living to 70 years of age free of chronic diseases. After up to 30 years of follow-up, 9,771 (9.3%) of 105,015 participants (66% women, mean age = 53 years (s.d. = 8)) achieved healthy aging. For each dietary pattern, higher adherence was associated with greater odds of healthy aging and its domains. The odds ratios for the highest quintile versus the lowest ranged from 1.45 (95% confidence interval (CI) = 1.35–1.57; healthful plant-based diet) to 1.86 (95% CI = 1.71–2.01; Alternative Healthy Eating Index). When the age threshold for healthy aging was shifted to 75 years, the Alternative Healthy Eating Index diet showed the strongest association with healthy aging, with an odds ratio of 2.24 (95% CI = 2.01–2.50). Higher intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, legumes and low-fat dairy products were linked to greater odds of healthy aging, whereas higher intakes of trans fats, sodium, sugary beverages and red or processed meats (or both) were inversely associated. Our findings suggest that dietary patterns rich in plant-based foods, with moderate inclusion of healthy animal-based foods, may enhance overall healthy aging, guiding future dietary guidelines.
Similar content being viewed by others
Main
The US population of older adults has steadily increased in the past few decades; however, 80% of older adults have at least one chronic health condition, highlighting the complex health challenges facing this demographic shift1. Promoting healthy aging is a global priority1,2. This commitment is driven by the goal of promoting a high quality of life, supporting continued contribution to society and reducing healthcare costs. Diet is the first leading behavioral risk factor for noncommunicable diseases and mortality burden globally3, and the second after tobacco use in US older adults 4.
Recently, the World Health Organization acknowledged that prioritizing the preservation of functional ability and the prevention of capacity decline should be central to the model of healthy aging5. This shift moves away from the traditional disease-centric approach to aging, aiming to offer older adults enhanced care5. Intervention and observational studies have provided compelling evidence that a better-quality diet is beneficial for the prevention of cardiovascular disease6,7, type 2 diabetes8 and premature mortality9. Studies have also evaluated the effects or the associations of foods and nutrients with age-related cognitive and physical performance outcomes10,11 and depressive symptoms12,13,14. However, few studies have examined the association of dietary patterns with a multidimensional model of healthy aging15,16,17,18,19,20. Examining and contrasting dietary patterns in relation to healthy aging will inform public health recommendations aimed at fostering the overall health and well-being of older adults, encompassing cognitive, physical and mental health, and the prevention of chronic diseases.
In this study, we examined the association between long-term adherence to eight healthy dietary patterns, including the Alternative Healthy Eating Index (AHEI), Alternative Mediterranean Index (aMED), the Dietary Approaches to Stop Hypertension (DASH), the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND), the healthful plant-based diet (hPDI), the Planetary Health Diet Index (PHDI), the empirically inflammatory dietary pattern (EDIP), the empirical dietary index for hyperinsulinemia (EDIH) and ultraprocessed food (UPF) consumption, and healthy aging after 30 years in two large prospective US cohorts. We then examined these associations in specific subgroups, including stratification according to sex, ancestry, socioeconomic status (SES) and lifestyle factors. We also examined the associations of individual foods and nutrients contributing to such dietary patterns.
Results
Of 105,015 participants, 70,091 were women (NHS) and 34,924 were men (HPFS) (Fig. 1). After a follow-up of up to 30 years, 9,771 (9.3%) participants achieved healthy aging, 7,602 (10.8%) in the NHS and 2,169 (6.2%) in the HPFS. In the pooled cohorts, 39,769 (37.9%) reached the age of 70 years, 23,908 (22.8%) remained free of 11 chronic diseases, 35,555 (33.9%) maintained intact cognitive function, 29,543 (28.1%) maintained intact physical function and 27,842 (26.5%) maintained intact mental health.
The age-standardized characteristics of the study population are shown in Table 1 (pooled data) and in Extended Data Tables 1 and 2 (according to cohort). Participants in the highest energy-adjusted dietary pattern score quintile were more likely to have a higher SES, use multivitamins, have a higher level of physical activity and slightly lower body mass index (BMI); they were also less likely to have a history of depression compared to the lowest quintile. Participants in the highest quintile for the AHEI, MIND, hPDI, PHDI, reverse EDIH (rEDIH) and reverse EDIP (rEDIP) consumed more alcohol, while those in the highest quintile for DASH and aMED consumed less. While a higher proportion of participants were women in the highest quintile for aMED, PHDI, rEDIH and rEDIP, a higher proportion were men in the highest quintile for AHEI, DASH, MIND and hPDI. Extended Data Fig. 1 shows the Spearman correlations between all dietary pattern scores and UPF consumption.
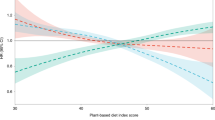
Higher adherence to all dietary patterns was associated with greater odds of healthy aging (Fig. 2 and Extended Data Table 3); components of the dietary patterns are shown in Fig. 3. The multivariable-adjusted odds ratios (ORs) (95% confidence intervals (CIs)) comparing the highest quintile to the lowest ranged from 1.45 (1.35–1.57; P < 0.0001) to 1.86 (1.71–2.01; P < 0.0001). The AHEI showed the strongest association followed by the rEDIH; the hPDI showed the weakest association. Based on the differences in ORs between pairs of scores and paired t-tests, the AHEI showed higher odds of healthy aging compared to the MIND, hPDI and rEDIP. The aMED, DASH, PHDI and rEDIH also demonstrated higher odds of healthy aging compared to the hPDI (Fig. 2). Using dietary pattern scores modeled as continuous variables, the associations with healthy aging were also the strongest for the AHEI and the weakest for the hPDI (Extended Data Table 3). The OR (95% CI) per standardized unit increase (representing the increment between the 10th and 90th percentiles) ranged from 1.40 (1.32–1.49) to 1.71 (1.60–1.82). Absolute risks, calculated based on the healthy aging prevalence and adjusted ORs, indicated 8.4% to 12.4% chances of achieving healthy aging among individuals with higher adherence to the dietary patterns (Extended Data Table 4).
In the main pooled dataset (n = 105,015), the average dietary pattern scores were calculated from 1986 to 2010. The forest plots show the ORs comparing Q5 to Q1 for each of the dietary patterns (visually represented by the centers of the error bars), the 95% CIs (visually represented by the error bars) and E values and their lower bound. Logistic regressions were used to estimate ORs and were adjusted for age at baseline (1986), cohort (sex), BMI (kg m−2), ancestry (European, Asian, African-American, Other), smoking status (never, former, current smoker: 1–14 cigarettes per day, 15–24 cigarettes per day and ≥25 cigarettes per day), alcohol intake (g per day) (for DASH, hPDI, PHDI), physical activity (MET-h week−1), multivitamin use ever (yes/no), family history of myocardial infarction (yes/no), family history of type 2 diabetes, family history of cancer, family history of dementia (yes/no), postmenopausal status (yes/no) and menopausal hormone use (no, past or current hormone use; only women), SES at baseline, marital status (yes/no), living alone ever (yes/no) and history of depression (yes/no) in the pooled cohorts. rEDIH and rEDIP are reversed scores to allow comparison with other scores. All two-sided P < 0.0001. The heatmaps show the OR difference between all pairs of scores. Positive differences are denoted in green and negative differences in pink; a darker color indicates a greater difference. *Two-sided P < 0.05 based on a paired t-test comparing ORs (not adjusted for multiple comparisons).
Pink: lower points or negative weights were assigned to higher intakes for this dietary factor; green: higher points or positive weights were assigned to higher intakes for this dietary factor; gray: higher points or positive weights were assigned to moderate intake. The EDIH and EDIP are presented as reversed scores to allow for comparison with other dietary scores.
When examining associations with each healthy aging domain, higher adherence to all dietary patterns was associated with all individual domains (Fig. 2 and Extended Data Table 3). The significant multivariable-adjusted ORs (95% CIs) comparing the highest quintile to the lowest ranged from 1.22 (1.15–1.28; P < 0.0001) to 1.65 (1.57–1.74; P < 0.0001) for intact cognitive health, with the PHDI showing the strongest association and the hPDI showing the weakest association. For intact physical function, the ORs (95% CIs) ranged from 1.38 (1.30–1.46; P < 0.0001) to 2.30 (2.16–2.44; P < 0.0001), with the AHEI showing the strongest association and the rEDIP showing the weakest association. For intact mental health, the ORs (95% CIs) ranged from 1.37 (1.30–1.45; P < 0.0001) to 2.03 (1.92–2.15; P < 0.0001), with the AHEI showing the strongest association and the hPDI showing the weakest association. For being free of chronic diseases, the ORs (95% CIs) ranged from 1.32 (1.25–1.40; P < 0.0001) to 1.75 (1.65–1.87; P < 0.0001), with the rEDIH showing the strongest association and the hPDI showing the weakest association. For surviving to the age of 70 years, the ORs (95% CIs) ranged from 1.33 (1.26–1.41; P < 0.0001) to 2.17 (2.05–2.30; P < 0.0001), with the PHDI showing the strongest association and the hPDI showing the weakest association.
Figure 4 illustrates the associations between individual dietary factors and healthy aging and its individual domains. While higher intakes of fruits, whole grains, vegetables, added unsaturated fats, nuts, legumes and low-fat dairy were associated with greater odds of healthy aging, higher intakes of trans fats, sodium, total meats, and red and processed meats were associated with lower odds. These foods or nutrients were also consistently associated with each healthy aging domain. Added unsaturated fat intake, including polyunsaturated fatty acids, was particularly associated with surviving to the age of 70 years, and intact physical and cognitive functions.
Each heatmap square represent the OR comparing the 90th to the 10th percentile for each of the dietary factors. Logistic regressions were used to estimate ORs and were adjusted for age at baseline (1986), cohort (sex), BMI (kg m−2), ancestry (European, Asian, African-American, Other), smoking status (never, former, current smoker: 1–14 cigarettes per day, 15–24 cigarettes per day and ≥25 cigarettes per day), alcohol intake (g per day), physical activity (MET-h week−1), multivitamin use ever (yes/no), family history of myocardial infarction (yes/no), family history of type 2 diabetes, family history of cancer, family history of dementia (yes/no), postmenopausal status (yes/no) and menopausal hormone use (no, past, or current hormone use; women only), SES at baseline, marital status (yes/no), living alone ever (yes/no) and history of depression (yes/no) in the pooled cohorts. ORs greater than 1.0 are denoted in green; ORs below 1.0 are denoted in pink; a darker color indicates a stronger association. *Two-sided P values corrected for multiple comparisons using a false discovery rate (FDR) < 0.05.
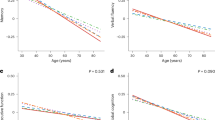
While adherence to all dietary patterns was significantly associated with healthy aging in both men and women, the associations were stronger in women (P interaction: 0.0226 to <0.0001; Fig. 5) except for rEDIH and rEDIP (no interaction). The associations were also stronger in smokers (for AHEI, aMED, DASH, MIND, hPDI; P interaction 0.047 to <0.0001), in participants with a BMI greater than 25 kg m−2 (for AHEI, MIND, hPDI, rEDIH, rEDIP; P interaction 0.042 to <0.0001) and in participants with a physical activity level below the median (for AHEI, aMED, DASH, MIND, hPDI, PHDI, rEDIP; P interaction 0.038 to <0.0001; Fig. 5). A significant interaction between SES and rEDIH (P interaction = 0.013) and rEDIP (P interaction = 0.017) was observed. No interaction was found for ancestry (European versus non-European).
The forest plots show the ORs comparing the 90th to the 10th percentile for each of the dietary patterns (visually represented by the centers of the error bars) and 95% CIs (visually represented by error bars). Logistic regressions were used to estimate the ORs and were adjusted for age at baseline (1986), cohort (sex), BMI (kg m−2), ancestry (European, Asian, African-American, Other), smoking status (never, former, current smoker: 1–14 cigarettes per day, 15–24 cigarettes per day and ≥25 cigarettes per day), alcohol intake (g per day), physical activity (MET-h week−1), multivitamin use ever (yes/no), family history of myocardial infarction (yes/no), family history of type 2 diabetes, family history of cancer, family history of dementia (yes/no), postmenopausal status (yes/no) and menopausal hormone use (no, past, or current hormone use; women only), SES at baseline, marital status (yes/no), living alone ever (yes/no) and history of depression (yes/no), excluding the stratified variable where applicable, in the pooled cohorts. ** two-sided P interaction <0.0001 (not adjusted for multiple comparisons). *Two-sided P interaction < 0.05 (not adjusted for multiple comparisons); sex, AHEI P = 0.022; MIND P = 0.001; hPDI P = 0.002; PHDI P = 0.0008; BMI, AHEI P = 0.001; MIND P = 0.024; and hPDI P = 0.015. For physical activity, DASH P = 0.0003; hPDI P = 0.0005; rEDIP P =0.023. For smoking, AHEI P = 0.005; aMED P = 0.010; MIND P = 0.0007; hPDI P = 0.002. For SES, rEDIH P = 0.019; rEDIP P = 0.023.
Secondary analyses showed consistency with the main results. When using a higher age cutoff of 75 years, the AHEI also showed the strongest association (Extended Data Table 5). When applying linear weights to dietary pattern scores, results were consistent with the main analysis (Extended Data Table 6).
Higher UPF consumption (comparing the highest quintile to the lowest) was associated with 32% lower odds of healthy aging (95% CI = 27–37%; Extended Data Table 7). Higher consumption of UPFs was also associated with lower odds of maintaining intact cognitive function, physical function and mental health, living free of chronic diseases and reaching the age of 70 years (Extended Data Table 7).
Discussion
In two large prospective cohorts of US women and men, we found that higher adherence to dietary patterns, namely the AHEI, aMED, DASH, MIND, hPDI, PHDI, rEDIP and rEDIH, during mid-life was associated with greater odds of healthy aging after a 30-year follow-up. Among dietary patterns, AHEI was the most strongly associated with healthy aging and hPDI was the least associated. Compared to participants in the lowest quintile, those who were in the highest AHEI quintile (energy-adjusted mean score = 68.6 ± 4.6) had 86% greater odds of achieving healthy aging using an age cutoff of 70 years and 2.24 times greater odds using an age cutoff of 75 years. The AHEI was closely followed by the rEDIH, aMED, DASH, PHDI, MIND, rEDIP and lastly the hPDI. Associations were independent of other lifestyle factors, including physical activity level, smoking and BMI. The AHEI was also the most strongly associated with maintaining intact physical function and mental health among individual healthy aging domains. The PHDI was most strongly associated with maintaining intact cognitive health and surviving to the age of 70 years. The rEDIH was the most strongly associated with being free of chronic diseases. A higher intake of UPFs was inversely correlated with higher diet quality scores and was also associated with lower odds of healthy aging. Our findings provide evidence to support that adherence to healthy dietary patterns represents a potential strategy for healthy aging, patterns that particularly are richer in fruits, vegetables, whole grains, unsaturated fats, nuts and legumes, that include some dairy products, and that are lower in trans fats, sodium, and red and processed meats.
While all dietary patterns share similarities such as promoting an intake of fruits, vegetables and whole grains, while reducing the amount of red and processed meats, each pattern emphasizes specific components. For instance, while the aMED diet focuses on the Mediterranean staples of olive oil, fish and nuts21, MIND further highlights the cognitive benefits of berries22. The DASH diet prioritizes sodium restriction for blood pressure control23, the PHDI emphasizes healthy low greenhouse gas emission foods, such as plant-sourced protein food24, and the hPDI uniquely attributes positive scoring to healthy plant-based foods and negative scoring to animal-derived foods25. In a previous report, adherence to the AHEI and aMED, assessed in 1984–1986, was associated with 34% (95% CI = 9–66%) and 46% (95% CI = 17, 83%) greater odds of healthy aging, respectively, in the NHS (n = 10,670; 15-year follow-up)19. This analysis examined two dietary patterns with healthy aging in 2000 using the same definition as in the current study, but the Telephone Interview for Cognitive Status was used to assess the cognitive health domain. Our analysis, which included both the NHS and HPFS, involved long-term dietary assessment of eight dietary patterns over a period of 14 years, with an assessment of healthy aging conducted 30 years after baseline. The results showed consistent and stronger associations for these two scores (84% greater odds for AHEI and 62% for aMED). The association between dietary patterns and healthy aging was also examined in other populations, namely in France16, Australia17,18, China15 and Israel20, and corroborated our findings. In the SUpplementation en VItamines et Minéraux AntioXydants study (n = 3,012, 38% healthy agers, 13-year follow-up) and Singapore Chinese Health Study (SCHS) (n = 14,159, 20% healthy agers, 20-year follow-up), higher adherence to a Mediterranean-style diet was associated with 36% (95% CI = 12–65%; tertile 3 versus tertile 1) and 53% (95% CI = 35–73%; quartile 4 versus quartile 1) greater likelihood of achieving healthy aging, respectively. The AHEI, HEI 2015 and adherence to the Australian National Dietary Guidelines were similarly associated with healthy aging with ORs ranging from 1.34 to 1.73 in the SCHS, the Israeli National Health and Nutrition Survey of Older Adults (n = 1,770, 13.7% healthy agers; 40% excluding deaths; median follow-up of 12.6 years) and the Blue Mountains Eye Study (n = 1,609, 15.5% healthy agers, 10-year follow-up). Among the dietary patterns also examined in other cohorts, we found significant interactions between sex and DASH, aMED, AHEI and hPDI; between physical activity level and the AHEI, aMED and hPDI; between smoking and the AHEI, aMED, DASH and hPDI; and between BMI and the AHEI and hPDI. Differences in the study populations regarding sex, lifestyle factors and BMI may explain the variations observed in the ORs across studies. The methods for assessing diet varied across studies, as did the definitions of healthy aging. Differences included age cutoffs, questionnaires or measures used for assessing domains, consideration of chronic diseases and the inclusion or exclusion of additional clinical measures. Moreover, some studies excluded deceased individuals from the sample population, potentially resulting in varying proportion of healthy agers and discrepancies in the classification of healthy agers. Standardization of a composite healthy aging outcome is warranted to allow proper comparison of research studies; deaths should be considered as usual agers and be included in the analyses to avoid selection bias.
Using a data-driven approach, Hodge et al.18 discerned four dietary patterns that were associated with healthy aging in the Melbourne Collaborative Cohort Study (n = 6,308, 18.6% healthy agers; median follow-up of 11.7 years for survivors). The dietary pattern that showed the strongest positive association with healthy aging predominantly consisted of fruits, whereas the pattern inversely associated with healthy aging primarily featured red meat. Assman et al.16 examined the individual dietary factors of the Mediterranean-style diet and their association with healthy aging in the SUpplementation en VItamines et Minéraux AntioXydants cohort and found a higher intake of fruits and vegetables to be favorably associated with healthy aging, and meat and alcohol to be unfavorably associated16. These findings agree with our results showing that a higher intake of fruits (overall and berries) and vegetables (overall, leafy green and dark yellow) was associated with greater odds of healthy aging, whereas a higher intake in trans fats, sodium, meats (total, red and processed and unprocessed) and liquor was associated with lower odds of healthy aging. In the Blue Mountains Eye Study, Gopinath et al.26 only found an association for fruits (healthy aging OR = 1.57, 95% CI = 1.06–2.34; quartiles 2 + 3 versus quartile 1; not significant for quartile 4 versus quartile 1) among the individual dietary factors examined. In the current study, most of the individual foods associated with healthy aging were consistently associated with the healthy aging domains individually, except for a few including fast and fried foods away from home, and snacks, which were positively associated with surviving to the age of 70 years. Although the consumption of fried food has been associated with an increased risk of cardiovascular events, evidence suggests no association with an all-cause mortality risk. The social aspect related to eating away from home may explain part of the association with living to the age of 70 years27, although more research in this area is needed to explain these associations.
Our findings showed that each dietary pattern examined was associated with each specific individual component of healthy aging. One prospective study also examined associations of dietary patterns, specifically the aMED, DASH, AHEI, PDI and hPDI, with the healthy aging domains15. Consistent with our results, Zhou et al.15 found significant associations between the aMED, DASH, AHEI and hPDI, and maintaining intact cognitive function; AHEI and DASH for staying free of chronic diseases; aMED, DASH, AHEI, hPDI and PDI for maintaining physical function and mental health (no clinical depression) in the SCHS study. However, no association was found between aMED, PDI and hPDI and the chronic disease component, and the PDI and the cognitive function component. Extensive evidence from intervention and observational studies supports that higher adherence to healthy dietary patterns is protective or associated with a lower risk of chronic diseases28. There is also accumulating evidence supporting the association of dietary patterns and dietary factors with mental, physical and cognitive health (reviewed in refs. 29,30). Beyond traditional measures of chronological age or disease burden, healthy aging is multifaceted as recognized by the World Health Organization in their first World report on ageing and health31. While examining domains in isolation provides more targeted insights into the potential mechanisms, investigating healthy aging as a multi-component outcome may inform holistic health strategies32. Our findings allow us to capture the multidimensional nature of aging and evaluate dietary patterns and food intake associations comprehensively.
Strengths of this study include the prospective design and large population size for robustly powered analyses. Repeated measurements of diet, body weight and lifestyle variables enabled us to consider long-term adherence to healthy dietary patterns and potential confounding factors, and mitigate random measurement errors. The long 30-year follow-up allowed the examination of the mid-life diet and its association with healthy aging in later life. Nevertheless, the results of this study need to be interpreted in the context of its limitations. First, although a lag of 6 years between the last diet update and healthy aging assessment was considered, reverse causation cannot be completely excluded. While it is plausible that higher adherence to healthy diets could be indicative of a higher SES and overall healthy lifestyle, our results remained consistent after accounting for such factors. However, residual confounding may still exist because of other unmeasured factors, such as environmental influences, although the E values indicate that our results are robust to potential confounding. Also, the cognitive and physical function domains were assessed using validated self-reported questionnaires instead of objective measurements, which limits in-depth assessment and classification. Lastly, our population included health professionals, which may limit the generalizability of our results. Replicating the analyses in populations with diverse SES and ancestries would offer further insights into their generalizability.
Greater long-term adherence to a healthy diet during mid-life was associated with greater odds of healthy aging and of its individual domains in US adults. Among the eight dietary patterns examined in this study, a diet that was developed to predict chronic disease risk as measured by the AHEI may confer the highest benefit for healthy aging in both men and women. Beyond the prevention of chronic disease, our findings extend recommendations to promote overall healthy aging, encompassing cognitive, physical and mental health.
Methods
Study population
Analyses were performed in the NHS and HPFS. The NHS was established in 1976 and included 121,700 US female registered nurses aged 30–55 years33. The HPFS was initiated in 1986 and recruited 51,525 male health professionals aged 40–75 years34. Details about the cohorts were published previously33,34. Biennial assessments of lifestyle factors and medical history were conducted through mailed questionnaires, maintaining a follow-up rate exceeding 90%. High validity and reproducibility of self-reported health information in the cohorts has been reported previously35,36,37. For both cohorts, the baseline for this analysis was 1986, that is, when the food frequency questionnaires (FFQ) allowed for computing all dietary pattern scores.
Figure 1 shows the flow diagram of the study. Participants included in this analysis had answered the 1986 questionnaires and had a chance of attaining 70 years at the end of the follow-up (aged between 39 and 69 years at baseline; n = 9,920 excluded). Participants with a history of one or more of 11 major chronic diseases, including cancer (except for non-melanoma skin cancers), diabetes, myocardial infarction, coronary artery disease, congestive heart failure, stroke, kidney failure, chronic obstructive pulmonary disease, Parkinson disease, multiple sclerosis and amyotrophic lateral sclerosis, at baseline (n = 8,953), with missing data for one or more dietary pattern scores between 1986 and 2010, or who reported implausible total energy intakes (<500 or >3,500 kcal d−1 for women and <800 or >4,200 kcal d−1 for men) (n = 15,016) and with missing healthy aging phenotype (n = 34,321) were excluded.
The study protocol was approved by the institutional review boards (IRBs) of the Brigham and Women’s Hospital (BWH), Harvard T.H. Chan School of Public Health (HSPH) and participating registries (IRB protocol nos. 2001P001945/BWH and 10372) as required. Per long-standing IRB-approved procedures at BWH and HSPH, the completion and return of the baseline and subsequent follow-up questionnaires implies consent. Before 2006, consenting practices varied and many collections were conducted with implied consent. A waiver of documentation for informed consent was granted for these studies. Written informed consent was required for medical record acquisition.
Dietary assessment
Dietary intake was measured using a validated FFQ with more than 130 items administered in 1986 and every 4 years thereafter. The validity and reliability of the FFQ for measuring nutrient, food and food group intakes have been reported previously38,39. Participants were asked how frequently they consumed specific foods in the past 12 months. Nutrients were calculated using the United States Department of Agriculture (USDA) and Harvard University Food Composition Databases40, and supplemented with biochemical analyses. Based on the reported nutrient and food intakes, eight dietary pattern scores were computed, including the AHEI, aMED, DASH, MIND, hPDI, PHDI, EDIP and EDIH, as well as UPF consumption. The AHEI, aMED, DASH, MIND, hPDI, and PHDI scores, and UPF consumption, have been developed based on dietary recommendations and available evidence. The scores showed moderate-to-high validity and reproducibility41 and were associated with risk of health outcomes28,42,43,44. The EDIP and EDIH were empirically derived using biomarkers of chronic inflammation45 and hyperinsulinemia46, respectively.
The AHEI score was computed based on the intake of 11 foods and nutrients that have been positively or inversely associated with chronic disease risk, including fruits, vegetables, nuts and legumes, alcohol, red and processed meat, whole grains, sodium, trans fats and long-chain n-3 (omega-3) fatty acids47. Each component was scored on a scale from 0 to 10 and the AHEI ranged from 0 to 110, a higher score indicating better overall diet quality. Adherence to the Mediterranean diet was assessed using a modified version of the 9-point aMED score21. The score was calculated based on adherence to nine food items (with either higher or lower intake) that characterize the Mediterranean diet: vegetables; legumes; fruits; nuts; whole grains; fish; moderate alcohol consumption; lower intake of red and processed meat; and monounsaturated to saturated fatty acids21. The modified aMED score ranged from 0 to 9, a higher score denoting a higher adherence to the Mediterranean diet21. The DASH score, designed to help prevent or treat hypertension, was based on eight dietary factors, including intake of high fruits, vegetables, nuts and legumes, low-fat dairy products, whole grain intake, low sodium, sweetened beverages and processed and unprocessed red meats23. Each component was attributed a score between 0 and 5 based on intake distribution quintiles. The overall score ranged from eight (lowest adherence) to 40 (highest adherence). The MIND score included ten brain-healthy dietary factors, including leafy-green vegetables, other vegetables, berries, nuts, whole grains, fish, beans, poultry, wine (in limited amounts) and olive oil, and five less healthy factors, including butter and margarine, cheese, red meat, fast/fried foods, and pastries and sweets22. Points of 0, 0.5 or 1 were attributed to each and the total MIND score ranged from 0 to 15, a higher score indicating a higher adherence. The hPDI was designed to reflect adherence to a healthy plant-based diet48; it included 18 dietary factors and ranged from 18 (lowest adherence) to 90 (highest adherence). The PHDI was derived based on the adherence to the reference diet included in the EAT-Lancet report49. The reference diet was based on evidence for health outcomes and staying within planetary boundaries for greenhouse gas emissions and other environmental parameters24. The scoring criteria included 15 dietary factors. For each dietary factor, the score ranged from 0 to 10, except for non-soy legumes and soy foods, which contributed a maximum score of 5. The total PHDI score ranged from 0 (non-adherence) to 140 (perfect adherence). The EDIP was scored based on 18 dietary factors related to inflammation50. The EDIH included 18 dietary factors related to hyperinsulinemia46. Given that higher EDIH and EDIP scores denote higher hyperinsulinemia and inflammatory dietary patterns, respectively, the orientation of the scores were reversed to ease comparison with other dietary scores and were denoted as rEDIH and rEDIP. Figure 3 is a visual representation of the dietary patterns and their dietary factors.
Food items were also categorized according to the NOVA classification system51. The average daily energy intake from UPFs was calculated, and the percentage of total daily energy from UPFs was determined based on the average total energy intake.
Assessment of healthy aging
Based on the construct of ‘successful aging’ described by Rowe & Kahn52 and previous reports19,53,54,55,56, a healthy aging phenotype was defined as surviving to the age of 70 years without the presence of 11 major chronic diseases and with no impairment in cognitive function, physical function or mental health. Participants who did not meet the phenotype criteria or who died before 2016 were considered as usual agers. Those who died after 2016, but had a complete assessment of the phenotype were included in the analyses. Cognitive function was assessed using a validated Subjective Cognitive Decline questionnaire57 in which reporting one or fewer of seven (NHS) or six (HPFS) cognitive concerns was considered as intact cognitive function. Physical function was assessed using the 36-item Short Form survey58 subsection on physical limitations that includes ten questions. Participants who reported not being limited in climbing one flight of stairs, walking one block, walking more than a mile, vacuuming, moving a table, walking several blocks, bathing or dressing, and being a little or not limited in climbing several flights of stairs, running lifting, bending, kneeling stooping and lifting carrying groceries, were considered as having intact physical function. Mental health was evaluated using the 15-item Geriatric Depression Scale, which ranges from 0 to 15 with a lower score indicating fewer depressive symptoms59. Reporting 1 or fewer depressive symptom (median value of both cohorts) was considered as having intact mental health. The 11 major chronic diseases were selected as they are the primary causes of mortality in the United States60 or are considered to be highly debilitating. They were also those ascertained at baseline and throughout the follow-ups. Clinical diagnoses of the major chronic diseases were reported by participants or next of kin for the deceased and were then ascertained by a physician through medical records, pathology reports or supplemental questionnaire inquiries, which are highly valid in these cohorts61. In the NHS, cognitive function was assessed in 2014; the presence of chronic diseases, physical function and mental health were assessed in 2016. In the HPFS, all domains were assessed in 2016.
Assessment of covariates
Every 2 years, participants completed a questionnaire that queried on body weight, ancestry, smoking status, physical activity, multivitamin use ever, family history of chronic diseases, including myocardial infarction, type 2 diabetes, cancer and dementia, postmenopausal status and hormone use in women, marital status, living alone and history of depression (based on antidepressant medication use and self-report of depression). The questionnaires are available online at https://nurseshealthstudy.org/participants/questionnaires for the NHS and at https://www.hsph.harvard.edu/hpfs/hpfs-questionnaires/ for the HPFS. BMI was calculated by dividing the weight (kg) by the height (m2). SES was calculated as a composite score using the participant’s geocoded address, combining US census household income, home value, college degree, ancestry, occupied housing units and unemployment, and whether families were receiving interest or dividends62.
Statistical analysis
The follow-up duration was calculated from the date when the first FFQ was returned until the date of the participant’s death or the date of assessment for healthy aging in 2016, whichever occurred first. The main analysis used the average of available dietary pattern scores between 1986 and 2010 as the exposure to capture long-term intake and allow a lag of 6 years between exposures and outcomes. The residual method was used to adjust dietary pattern scores for total energy intake, including energy from alcohol63, and quintiles were calculated. Missing values for covariates were replaced with the cohort-specific median value. As outcomes are binary and measured at one time point, logistic regression models were used to estimate the ORs and 95% CIs of healthy aging and its individual domains according to quintiles of energy-adjusted dietary pattern scores, with age at baseline in 1986 as a covariate (base model). The multivariable-adjusted model was further adjusted for baseline-reported ancestry (European, Asian, African-American, Other), SES (composite score) and marital status (yes/no), ever used multivitamins (yes/no), ever lived alone (yes/no), family history of dementia (yes/no), myocardial infarction, cancer, and diabetes (yes/no), and medical history of depression (yes/no), diabetes and CVD (yes/no), smoking status in 2010 (never, former, current smoker: 1–14 cigarettes per day, 15–24 cigarettes per day and ≥25 cigarettes per day), postmenopausal status (yes/no) and menopausal hormone use (no, past, or current hormone use; women only), and mean (1986–2010) BMI (kg m−2), physical activity (MET-h week−1) and alcohol intake (g per day) for DASH, hPDI and PHDI. An OR above 1 indicated a higher likelihood of healthy aging. Associations using the patterns as continuous variables, standardized according to their respective increment from the 10th to the 90th percentiles, were also examined. Analyses were performed in each cohort and in the pooled cohorts. The analyses in the pooled cohorts were further adjusted for cohort (sex). Absolute risks in both quintiles were calculated using the proportion of healthy agers in Q1 and the multivariable-adjusted OR comparing Q5 versus Q1. E values and the lower or upper bound were calculated for the ORs to assess the potential impact of unmeasured confounding on the observed associations. A higher E value denotes stronger evidence that unmeasured confounding would be required to fully explain away the observed association. Prespecified subgroup analyses were conducted according to cohort (sex), BMI (<25 versus ≥25 kg m−2), physical activity (above/below median), smoking (yes/no), SES (above/below median) and ancestry (European/non-European). Potential subgroup interactions were evaluated using interaction models, including the product of the subgroup and the exposure. As secondary analyses, the association of dietary patterns scores with healthy aging using an age cutoff of 75 years, and the association of UPF consumption with healthy aging (>70 years) were assessed. As a sensitivity analysis, we applied linear weights to dietary pattern scores across seven time points, ranging from 1986 to 2010, assigning the highest weight to the year closest to the healthy aging assessment (2010) and the lowest weight to 1986.
Intake in the individual food groups and nutrients that reflect the dietary pattern scores were also energy-adjusted and standardized according to their respective increment from the 10th to the 90th percentiles. The associations of energy-adjusted food group and nutrient intakes with healthy aging and its domains were examined using logistic regressions, accounting for the covariates described in the multivariable-adjusted model. Given that all dietary factors are also found in the pattern scores, the models were not adjusted for any measure of diet quality. P values were corrected for FDR using the Benjamini–Hochberg method; an FDR-corrected P < 0.05 was considered statistically significant.
Analyses were performed with SAS v.9.4 (SAS Institute) and R v.4.2.0. Statistical tests were two-sided and P < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Because of participant confidentiality and privacy concerns, data are available only upon written request. According to standard controlled access procedures, applications to use the NHS and HPFS resources will be reviewed by our External Collaborators Committee for scientific aims, evaluation of the fit of the data for the proposed methodology and verification that the proposed use meets the guidelines of the Ethics and Governance Framework and the consent that was provided by the participants. Investigators can expect initial responses within 4 weeks of request submission. Further information, including the procedures for obtaining and accessing data from the NHS and HPSF is described at https://www.nurseshealthstudy.org/researchers (nhsaccess@channing.harvard.edu) and https://hsph.harvard.edu/research/health-professionals/resources/for-external-collaborators/. The USDA and Harvard University food composition databases are publicly available at https://www.fns.usda.gov/usda-fis/usda-foods-database and https://hsph.harvard.edu/department/nutrition/nutrition-questionnaire-service-center/#nutrient-data.
Code availability
The analysis code is publicly available through GitHub (https://github.com/DrTessier/diets_healthyaging/).
References
Centers for Disease Control and Prevention. Healthy Aging at a Glance, 2015: Helping People to Live Long and Productive Lives and Enjoy a Good Quality of Life https://stacks.cdc.gov/view/cdc/43961 (National Center for Chronic Disease Prevention and Health Promotion (U.S.) & Division of Adult and Community Health, 2015).
Office of Disease Prevention and Health Promotion. Healthy Aging https://health.gov/our-work/national-health-initiatives/healthy-aging#:~:text=Promoting%20health%20and%20preventing%20disease,live%20longer%20and%20stay%20healthy (OASH, 2023).
Afshin, A. et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 393, 1958–1972 (2019).
Mokdad, A. H. et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 319, 1444–1472 (2018).
Bautmans, I. et al. WHO working definition of vitality capacity for healthy longevity monitoring. Lancet Healthy Longev. 3, e789–e796 (2022).
Shan, Z. et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern. Med. 180, 1090–1100 (2020).
Guasch-Ferré, M. & Willett, W. C. The Mediterranean diet and health: a comprehensive overview. J. Intern. Med. 290, 549–566 (2021).
Forouhi, N. G., Misra, A., Mohan, V., Taylor, R. & Yancy, W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ 361, k2234–k2241 (2018).
English, L. K. et al. Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw. Open 4, e2122277–e21222295 (2021).
Scarmeas, N., Anastasiou, C. A. & Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet Neurol. 17, 1006–1015 (2018).
Tessier, A.-J. & Chevalier, S. An update on protein, leucine, omega-3 fatty acids, and vitamin D in the prevention and treatment of sarcopenia and functional decline. Nutrients 10, 1099–1115 (2018).
Nicolaou, M. et al. Association of a priori dietary patterns with depressive symptoms: a harmonised meta-analysis of observational studies. Psychol. Med. 50, 1872–1883 (2020).
Okereke, O. I. et al. Effect of long-term vitamin D3 supplementation vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA 324, 471–480 (2020).
Okereke, O. I. et al. Effect of long-term supplementation with marine omega-3 fatty acids vs placebo on risk of depression or clinically relevant depressive symptoms and on change in mood scores: a randomized clinical trial. JAMA 326, 2385–2394 (2021).
Zhou, Y.-F. et al. Association between dietary patterns in midlife and healthy ageing in Chinese adults: the Singapore Chinese Health Study. J. Am. Med. Dir. Assoc. 22, 1279–1286 (2021).
Assmann, K. E. et al. Association between adherence to the Mediterranean diet at midlife and healthy aging in a cohort of French adults. J. Gerontol. A Biol. Sci. Med. Sci. 73, 347–354 (2018).
Gopinath, B., Russell, J., Kifley, A., Flood, V. M. & Mitchell, P. Adherence to dietary guidelines and successful aging over 10 years. J. Gerontol. A Biol. Sci. Med. Sci. 71, 349–355 (2016).
Hodge, A. M., O’Dea, K., English, D. R., Giles, G. G. & Flicker, L. Dietary patterns as predictors of successful ageing. J. Nutr. Health Aging 18, 221–227 (2014).
Samieri, C. et al. The association between dietary patterns at midlife and health in aging: an observational study. Ann. Intern. Med. 159, 584–591 (2013).
Goshen, A. et al. Association of diet quality with longevity and successful aging in Israeli adults 65 years or older. JAMA Netw. Open 5, e2214916–e2214927 (2022).
Trichopoulou, A., Costacou, T., Bamia, C. & Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 348, 2599–2608 (2003).
Morris, M. C. et al. MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimers Dement. 11, 1007–1014 (2015).
Karanja, N. M. et al. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. J. Am. Diet. Soc. 99, S19–S27 (1999).
Bui, L. P. et al. Planetary Health Diet Index and risk of total and cause-specific mortality in three prospective cohorts. Am. J. Clin. Nutr. 120, 80–91 (2024).
Satija, A. et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J. Am. Coll. Cardiol. 70, 411–422 (2017).
Qin, P. et al. Fried-food consumption and risk of cardiovascular disease and all-cause mortality: a meta-analysis of observational studies. Heart 107, 1567–1575 (2021).
Björnwall, A., Mattsson Sydner, Y., Koochek, A. & Neuman, N. Eating alone or together among community-living older people—a scoping review. Int. J. Environ. Res. Public Health 18, 3495–3536 (2021).
Wang, P. et al. Optimal dietary patterns for prevention of chronic disease. Nat. Med. 29, 719–728 (2023).
Milte, C. M. & McNaughton, S. A. Dietary patterns and successful ageing: a systematic review. Eur. J. Nutr. 55, 423–450 (2016).
Yeung, S. S. Y., Kwan, M. & Woo, J. Healthy diet for healthy aging. Nutrients 13, 4310–4326 (2021).
Beard, J. R. et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet 387, 2145–2154 (2016).
Langevin, H. M., Weber, W. & Chen, W. Integrated multicomponent interventions to support healthy aging of the whole person. Aging Cell 23, e14001–e14045 (2024).
Bao, Y. et al. Origin, methods, and evolution of the three Nurses’ Health Studies. Am. J. Public Health 106, 1573–1581 (2016).
Rimm, E. B. et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet 338, 464–468 (1991).
Colditz, G. A. et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am. J. Epidemiol. 123, 894–900 (1986).
Rimm, E. B. et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1, 466–473 (1990).
Wolf, A. M. et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int. J. Epidemiol. 23, 991–999 (1994).
Gu, X. et al. Validity and reproducibility of a semiquantitative food frequency questionnaire for measuring intakes of foods and food groups. Am. J. Epidemiol. 193, 170–179 (2024).
Yuan, C. et al. Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women. Am. J. Epidemiol. 187, 1051–1063 (2018).
Nutrient Tables https://hsph.harvard.edu/department/nutrition/nutrition-questionnaire-service-center/ (Harvard T.H. Chan School of Public Health, 2025).
Yue, Y. et al. Reproducibility and validity of diet quality scores derived from food-frequency questionnaires. Am. J. Clin. Nutr. 115, 843–853 (2022).
Berendsen, A. M. et al. Association of long-term adherence to the MIND diet with cognitive function and cognitive decline in American women. J. Nutr. Health Aging 22, 222–229 (2018).
Shan, Z. et al. Healthy eating patterns and risk of total and cause-specific mortality. JAMA Intern. Med. 183, 142–153 (2023).
Fung, T. T. et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 168, 713–720 (2008).
Tabung, F. K. et al. An empirical dietary inflammatory pattern score enhances prediction of circulating inflammatory biomarkers in adults. J. Nutr. 147, 1567–1577 (2017).
Tabung, F. K. et al. Development and validation of empirical indices to assess the insulinaemic potential of diet and lifestyle. Br. J. Nutr. 116, 1787–1798 (2016).
Chiuve, S. E. et al. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 142, 1009–1018 (2012).
Satija, A. & Hu, F. B. Plant-based diets and cardiovascular health. Trends Cardiovasc. Med. 28, 437–441 (2018).
Willett, W. et al. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 393, 447–492 (2019).
Tabung, F. K. et al. Development and validation of an empirical dietary inflammatory index. J. Nutr. 146, 1560–1570 (2016).
Khandpur, N. et al. Categorising ultra-processed foods in large-scale cohort studies: evidence from the Nurses’ Health Studies, the Health Professionals Follow-up Study, and the Growing Up Today Study. J. Nutr. Sci. 10, e77–e91 (2021).
Rowe, J. W. & Kahn, R. L. Human aging: usual and successful. Science 237, 143–149 (1987).
Sun, Q. et al. Alcohol consumption at midlife and successful ageing in women: a prospective cohort analysis in the nurses’ health study. PLoS Med. 8, e1001090–e1001099 (2011).
Shi, H. et al. Sleep duration and snoring at midlife in relation to healthy aging in women 70 years of age or older. Nat. Sci. Sleep 13, 411–422 (2021).
Shi, H., Huang, T., Schernhammer, E. S., Sun, Q. & Wang, M. Rotating night shift work and healthy aging after 24 years of follow-up in the Nurses’ Health Study. JAMA Netw. Open 5, e2210450–e2210464 (2022).
Ardisson Korat, A. V. et al. Dietary protein intake in midlife in relation to healthy aging—results from the prospective Nurses’ Health Study cohort. Am. J. Clin. Nutr. 119, 271–282 (2024).
Molinuevo, J. L. et al. Implementation of subjective cognitive decline criteria in research studies. Alzheimers Dement. 13, 296–311 (2017).
Ware, J. E. & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 30, 473–483 (1992).
de Craen, A. J. M., Heeren, T. J. & Gussekloo, J. Accuracy of the 15-item geriatric depression scale (GDS-15) in a community sample of the oldest old. Int. J. Geriatr. Psychiatry 18, 63–66 (2003).
Xu, J., Murphy, S. L., Kochanek, K. D. & Arias, E. Mortality in the United States, 2021. NCHS Data Brief www.cdc.gov/nchs/products/databriefs/db456.htm (US Department of Health and Human Services, CDC & National Center for Health Statistics, 2022).
Sun, Q. et al. Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch. Intern. Med. 170, 194–201 (2010).
DeVille, N. V. et al. Neighborhood socioeconomic status and mortality in the Nurses’ Health Study (NHS) and the Nurses’ Health Study II (NHSII). Environ. Epidemiol. 7, e235–e241 (2022).
Willett, W. & Stampfer, M. J. Total energy intake: implications for epidemiologic analyses. Am. J. Epidemiol. 124, 17–27 (1986).
Acknowledgements
The NHS and HPFS are supported by grants from the National Institutes of Health (nos. UM1 CA186107, P01 CA87969, R01 HL034594, R01 HL088521, U01 CA167552 and R01 HL35464). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. A.-J.T. was supported by a Canadian Institutes of Health Research Postdoctoral Fellowship Award. A.A.K. was supported by a USDA Cooperative Agreement no. 58-8050-3-003 and the National Center for Advancing Translational Sciences (no. 1K12TR004384). J.L. was supported by National Institute of Diabetes and Digestive and Kidney Diseases (nos. R00DK122128 and R01AG087356). M.G.-F. was supported by a Novo Nordisk Foundation grant no. NNF23SA0084103. The funders had no role in the design and conduct of the study, data collection, management, analysis and interpretation, preparation, review or approval of the manuscript, and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
A.-J.T. and M.G.-F. had full access to all the study data and take responsibility for the integrity of the data and the accuracy of the data analysis. A.-J.T., M.G.-F. and F.B.H. designed the research. A.-J.T. conducted the analyses, prepared the tables and figures, and wrote the manuscript. All authors contributed to the interpretation of the results and critical revision of the manuscript for important intellectual content. All authors approved the final version of the manuscript. The corresponding author attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Competing interests
M.G.-F. is the principal investigator of a grant funded by the International Nut Council. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Eirini Trichia and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Michael Basson, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Pairwise Spearman correlations between energy-adjusted average (1986-2010) dietary pattern scores.
A. Pairwise Spearman correlations were applied in the pooled main dataset (n = 105,015). P values for all correlations are two-sided and <0.0001 (not adjusted for multiple comparisons); B. Pairwise Spearman correlations were applied in the pooled dataset excluded participants with missing UPF data (n = 104,635). P values for all correlations are two-sided and <0.0001 (not adjusted for multiple comparisons). AHEI, alternative healthy eating index; AMED, alternative Mediterranean diet index; DASH, Dietary approaches to stop hypertension; MIND, Mediterranean-DASH intervention for neurodegenerative delay diet; hPDI, healthful plant-based diet index; PHDI, planetary health diet index; EDIH, empirical dietary index for hyperinsulinemia; EDIP, empirical dietary inflammatory pattern. The rEDIH and rEDIP are reversed scores to allow for comparison with other dietary scores.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tessier, AJ., Wang, F., Korat, A.A. et al. Optimal dietary patterns for healthy aging. Nat Med 31, 1644–1652 (2025). https://doi.org/10.1038/s41591-025-03570-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-025-03570-5
This article is cited by
-
Whole diets, whole health
Nature Medicine (2025)
-
The best foods for healthy ageing ― and the worst
Nature (2025)
-
Nutrition research must go local
Nature Medicine (2025)